Orthopaedic implants are crucial for restoring the function, stability, and mobility of bones, and they can be made from materials such as metal, ceramic, polymer, or bioabsorbable compounds. Metals, particularly titanium and its alloys, are widely used in load-bearing applications like hip, knee, and spine surgeries due to their superior mechanical strength and biocompatibility. The surface characteristics of titanium implants play a key role in bone healing, with rough surfaces and specific pore sizes improving osseointegration, promoting bone cell adhesion and growth, and allowing new blood vessels to support bone ingrowth. Combining solid and perforated sections in titanium implants offers an ideal balance between mechanical strength and biological integration, making them especially suitable for spinal applications, where both stability and bone integration are critical for healing.
Our recent study published in the Journal of Orthopaedic Research explored the biocompatibility and osseointegration of multi-component titanium alloy (Ti-6Al-4V) implants, key aspects taken into account in the design of our VCFix implant.
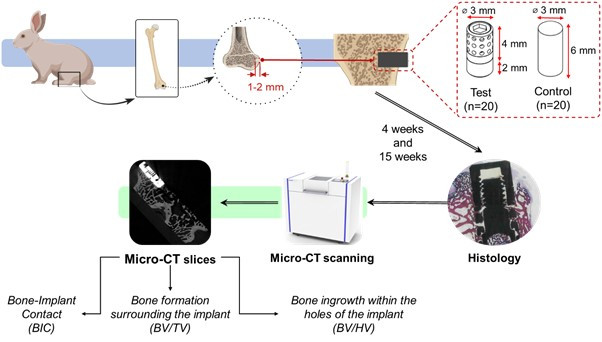
These implants, featuring a perforated design with high surface roughness, were compared to traditional smooth titanium implants in a rabbit model. The findings showed that the novel perforated implants demonstrated higher bone ingrowth and faster maturation of bone tissue, while also displaying minimal inflammatory response. After 15 weeks, the perforated implants exhibited better integration with the surrounding bone than the control group.
The study used micro-CT scans and histopathological analysis to assess bone-implant contact and bone formation. Results showed that bone ingrowth occurred more extensively within the perforated implants, promoting stronger mechanical interlocking with surrounding bone tissue. Additionally, the rough surface of the perforated implants improved early stabilization, facilitating faster healing and maturation compared to the smooth, solid implants used as controls. Importantly, both implant types showed minimal adverse host reactions, underscoring the biocompatibility of
titanium alloys.
These findings highlight the potential of multi-component, perforated titanium implants for use in orthopaedic and spinal surgeries. The combination of a perforated design with high surface roughness provides mechanical strength while encouraging biological integration, making it an ideal solution for bone repair and regeneration. The study suggests that this multi-component implant design could improve patient outcomes by promoting faster recovery and enhancing long-term stability in load-bearing applications.
You can access the paper through this link: https://doi.org/10.1002/jor.25974